Here’s what happened.
About 10 days ago, my dad fell while he was alone in his assisted living unit. He was fine (miraculously), just a bit bruised. But they sent him to the ER to make sure he didn’t have a concussion or anything else.
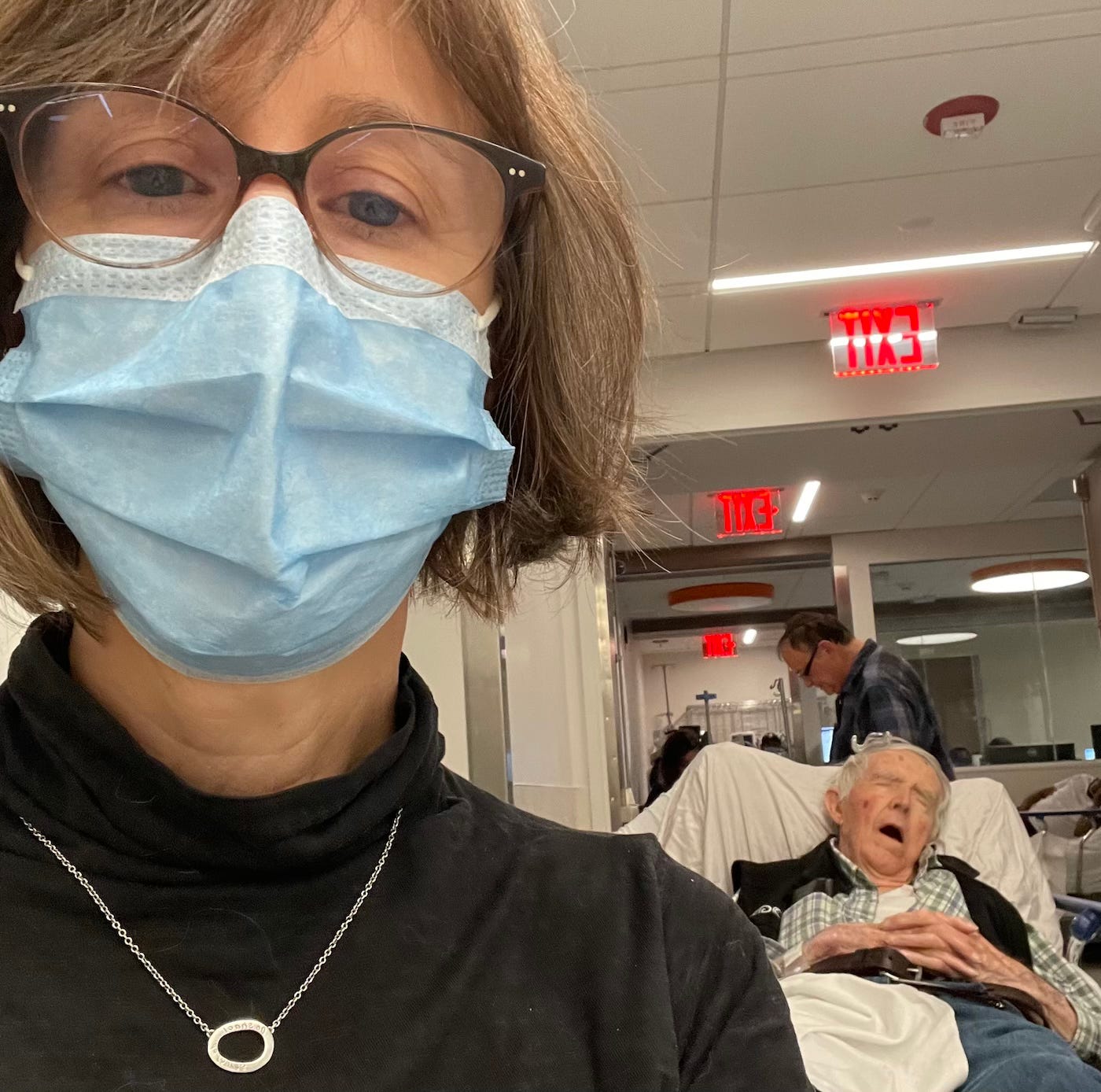
When I saw Dad in the ER that night, on a gurney in the hallway on top of so many others, and every device that could beep was, and the nurses squeezing past —
I thought, Here we go.
The risk of swallowing
You can predict what has happened since: Tests and more tests. Transferring Dad to a different branch of the hospital with a better geriatric team. X-Rays, MRIs, and blood work.
About four days into this quagmire, you’ll never guess what happened. (Wait, how did you guess?)
Dad got pneumonia because he aspirated a piece of food —
More tests. Oxygen. IV antibiotics. CT-scan. Then they take him off food for three days because of the risk of swallowing. (The risk of swallowing. Say that a few times.)
Dad is now in a fugue state, semi-conscious, largely unresponsive.
My brother and I are calling and texting the family. We can’t tell which way this is going.
Cellophane flowers of yellow and green
Imagine a merry-go-round with doctors on it. Forget the cute painted animals. The hospital is just a big, whirling platter with doctors and nurses and PAs, and PTs, and ETs, and FAs — and I’m just making it up at this point.
So you’re at the hospital, with this not-so-merry-go-round waltzing past, and you have to grab somebody —
Hahahahaha. Good luck! They are all available! But not when you’re available!
With persistence you get to talk to someone, or maybe they call you back? Does it matter? All the conversations turn, turn, turn, but for some reason you can’t form the words into what you’re trying to ask.
A string of pearls
Two young women show up and they are from the Volunteer squad. They work with the Delirium Team. [I am telling the truth here.]
They explain that the dramatic change in Dad’s state is not that he’s dying. Or not exactly. He’s slid into Delirium. It’s acute mental stress: a.k.a. too many shocks to the system when you’re 92 years old. Never mind the adult child of someone who is 92.
Luckily they have a pamphlet! We can keep the pamphlet. We are so grateful. No one has spent this much time talking to us. They are young and good and pure and wear matching dark-blue smocks.
When they offer to play Dad some soothing music via their hospital-issued iPad — and you say, Dad likes Glenn Miller — their eyes go wide. Glenn…what was that again?
We passed the School, where Children strove
Your brother and sister-in-law are optimistic. This could turn around. Could it? Six days ago Dad was more or less enjoying his new life at the assisted living place — Ok, not really — but now he’s eating a pureed diet and unable to form sentences.
Then: A doctor, maybe two, say something about transferring Dad to a rehab facility. To rehab what? you wonder.
Then: Someone else, another doctor, perhaps as old as 14 or 15, notes that people can live for years with dementia. Thank you! Is that the goal here?
Then a breakthrough on Day 8! You have a clarifying and cogent meeting with the Palliative Care Specialist. You ask for her name, and she spells it carefully, even though her name is not that unusual.
The next day, you ask the nurse — always someone you have never seen, yet sort of know — to please contact the palliative care specialist, whose name you have carefully remembered.
The nurse asks you for the name again. The nurse says she cannot find this person in the Care Chart.
She shows you the Care Chart on her very large screen, which is perched atop a wheely cart. Also: she has straws in case you need them.
And it’s true. The palliative care specialist is not listed.
But that’s her name, you say. I spoke with her.
I know, but she’s not on the Care Chart, the nurse says.
She is young, maybe the youngest of all the nurses. You sense her unease. And you’re aware that you could be approaching a line where things become hostile accidentally.
Ok, you say. Ok.
You google the palliative care specialist when you get home, and she does exist. But in another state, in another hospital system. Then, a subsequent listing shows her in the hospital where you met.
Of course. The discrepancies in the space-time continuum also impact health care!
This is why, when people ask you how you are, it’s really hard to explain.
If the spirit moves you, because I do think nomenclature matters even if civil discourse has taken a nosedive, pls email support@substack.com to request that they add Aging or at least Retirement as a category for content here. <3
Some stuff I read/watched/ate this week:
Marcus Aurelius: Meditations [I like this edition]
Pink Floyd: Echoes
Modern Family, S1, eps 5 - 14
Stella D’oro Swiss Fudge Cookies (all of them)
Tara Brach: Letting Go of Controlling, Pt. 1
Empty Boats [I memorized this as a child, and it came back to me today]